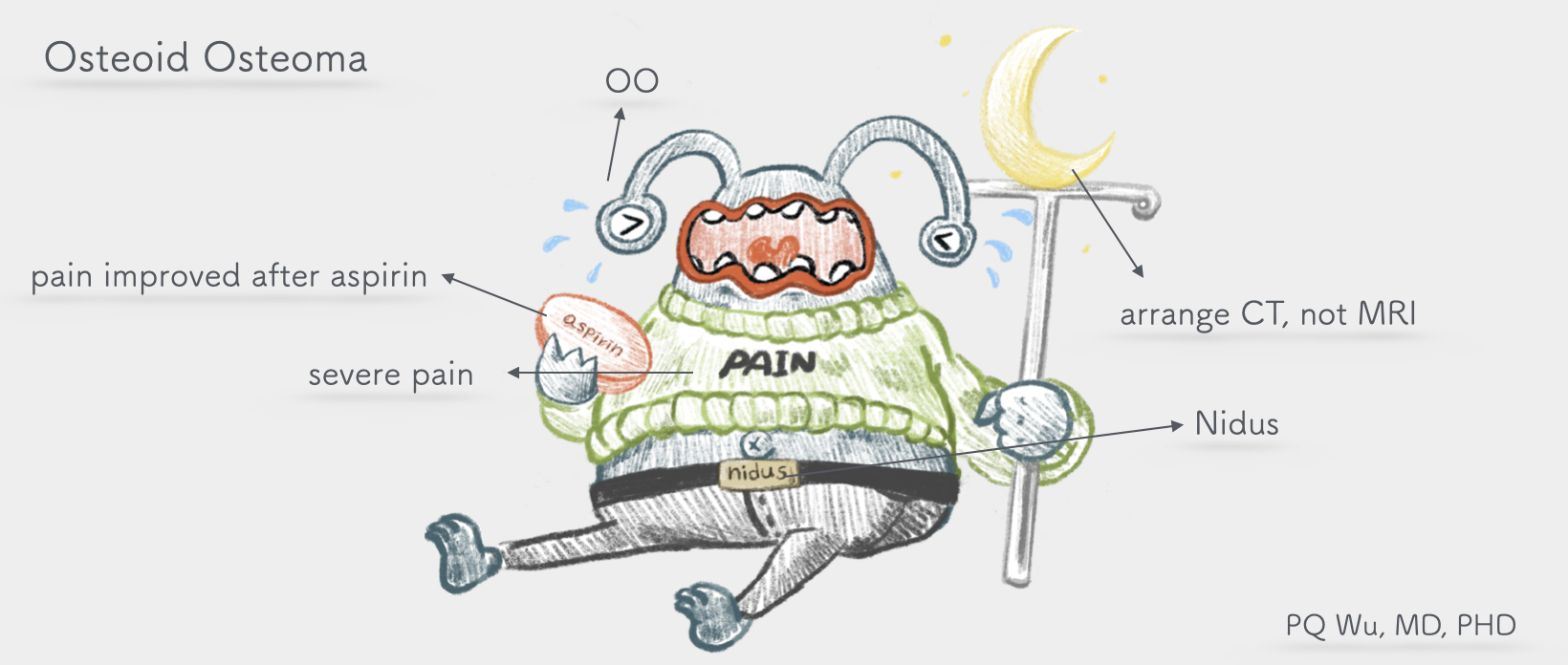
Osteoid osteoma is a rather peculiar tumor. The tumors are often less than a centimeter in size and quite small. As a result, the tumor is often unable to be discovered and diagnosed properly even after X-ray scanning. However, osteoid osteoma, although small, can cause extreme discomfort, especially during resting or sleeping at night, and even wake up patients because of pain! The most typical phenomenon is that when a patient takes painkillers or aspirin, the pain releases immediately! Sometimes when we hear a patient's complaint like this, we suspect that it may be an osteoid osteoma.
Chinese: None
English: None
The symptom of osteoid osteoma is 'pain', and it's a rather 'deep' and 'sore' discomfort. Especially in the middle of the night, patients are more likely to feel uncomfortable since their cortisol secretion is low! Worse, since it's relatively hard to diagnose the tumor, most patients experience pain in a considerable amount of time. According to the literature report, patients would have average of 11.8 months to 36 months of pain before being correctly diagnosed and treated. It's a very tough time!
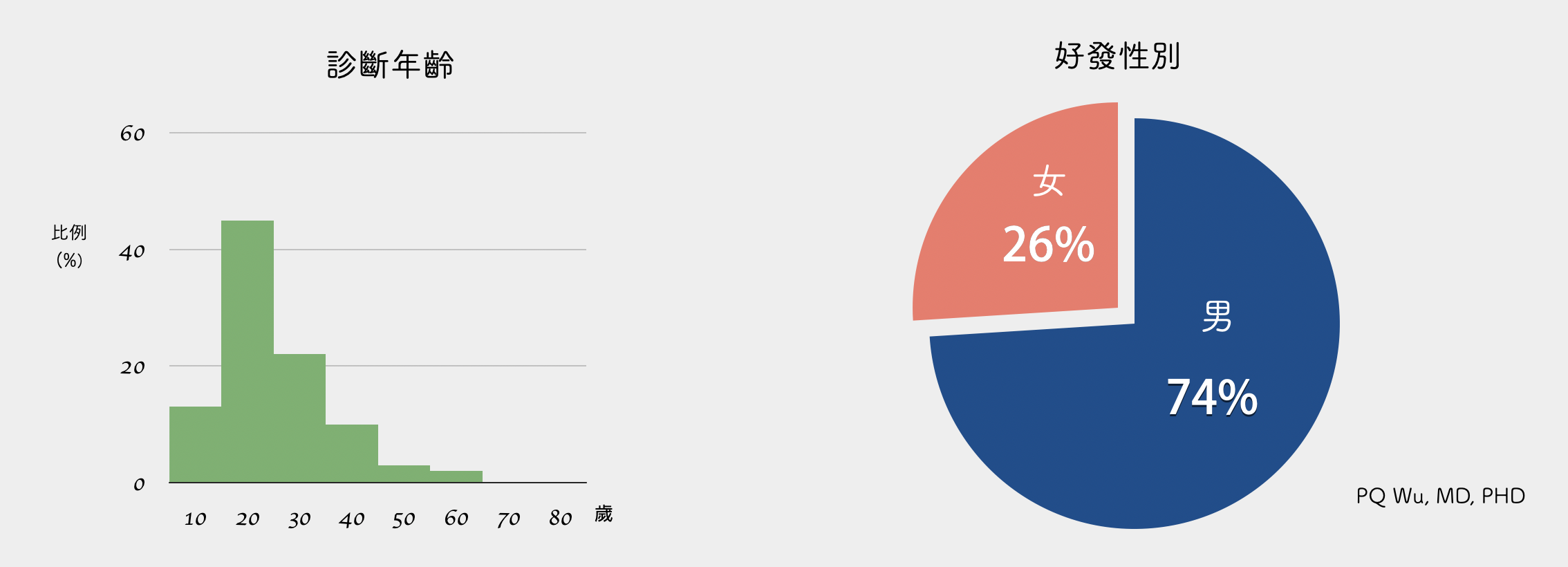
Osteoid osteoma is a rare benign bone tumor, taking about 10% of all benign bone tumors and 4% of all bone tumors. An outpatient clinic would discover a new patient in about two or three months at our Therapeutical and Research Center of Musculoskeletal Tumor in Taipei Veterans General Hospital. It is relatively uncommon in all benign bone tumors.
Osteoblastoma is much more likely to occur in men, accounting for about 75%. Most of these occur in adolescents between the ages of 10 and 30.
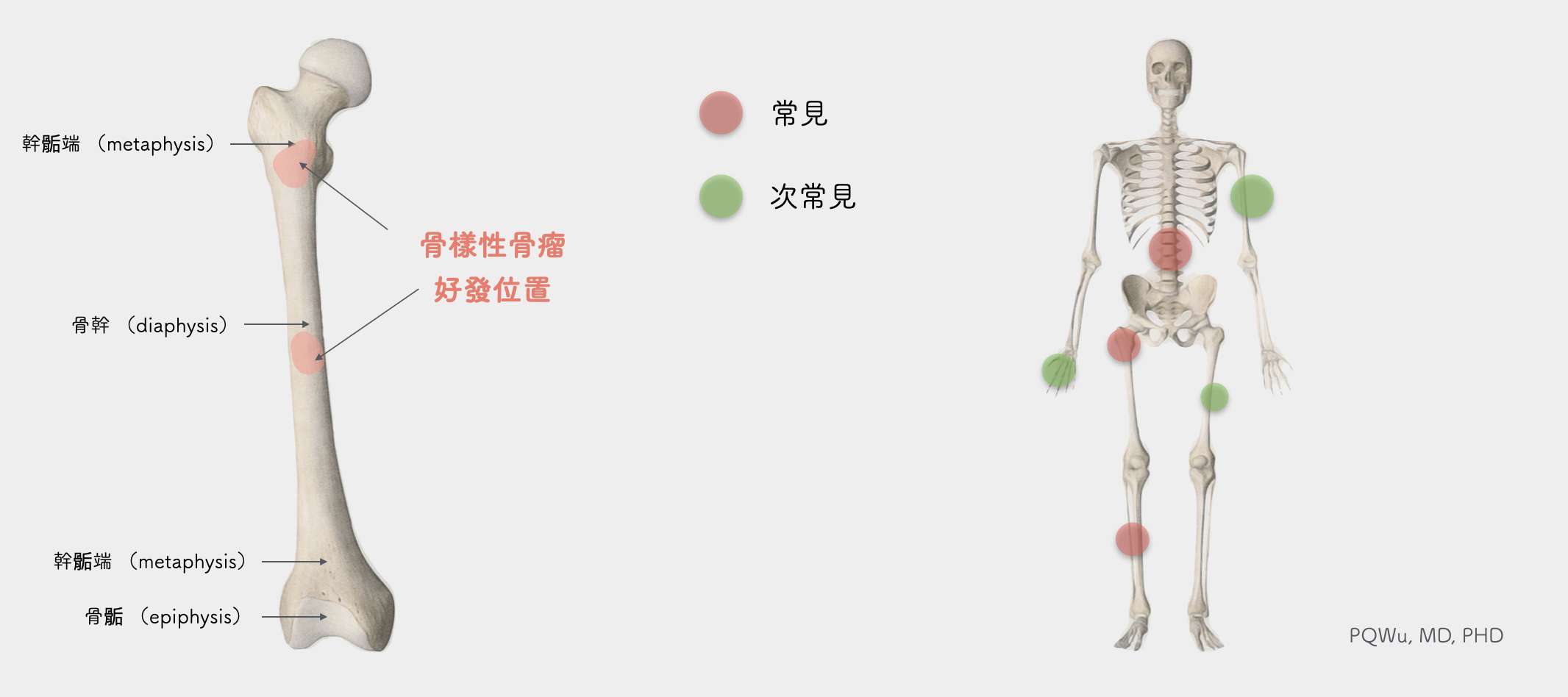
Osteoid osteoma occurs mostly in the femur and tibia. In addition, it occasionally occurs in the spine. Osteoid osteoma that occurs in the spine usually causes scoliosis due to pain. Medically, we divide the bones into epiphysis, metaphysis, diaphysis, and osteoid osteoma, which mostly occur at both ends of the backbone and differ from normal bone tumors.
The cause of osteoid osteoma is still unknown.
Imaging diagnosis for osteoid osteoma is quite difficult and requires considerable experience to drive correct diagnosis. In general, very noticeable bone sclerosis (reactive sclerosis) could be observed near the tumor.
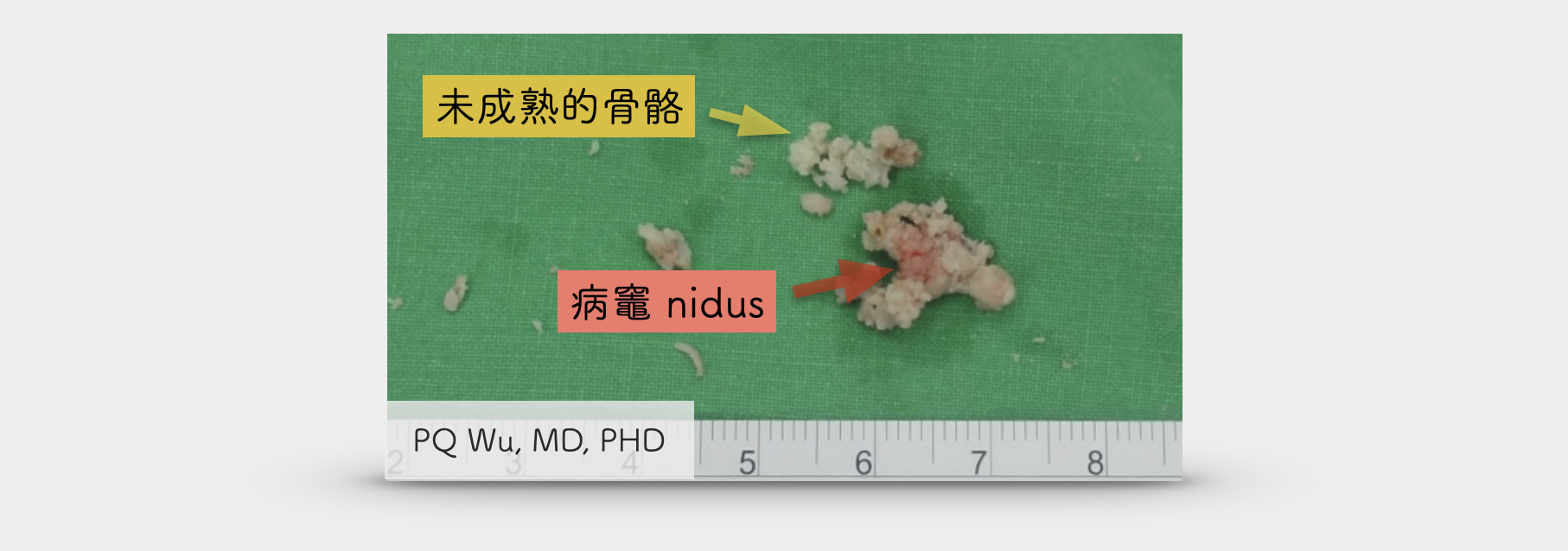
It looks like a bone-regenerating reaction after an injury. In some patients' X-ray images, we can see an unobtrusive cavity inside the bone sclerosis, that is, the actual location of the tumor. We call it 'Nidus'.
When we see nidus, we can diagnose it as osteoid osteoma. If we can't simply see nidus from X-ray images, we can help patients arrange a computer tomography (CT), and we shall be able to see it smoothly. Based on the location of the nidus, we can classify osteoid osteoma as cortical, medullary, and subperiosteal types.

One of the most bothering problems when diagnosing osteoid osteoma is conducting an MRI scan. Most physicians will infer some malignant bone tumors based on the abnormal findings they see on the bones and the reports of the patient having night pain. Such a rule to conduct an MRI examination works perfectly in every bone tumor except for the osteoid osteoma. It brings troubles to the physicians. Because in MRI examinations, not only is the 'lesions nidus' in osteoid osteoma sometimes invisible (because of the thinker cuts), but there is often an overly strong bone marrow edema or synovitis). These excessive reactions can lead the physician to misdiagnose osteoid osteoma as osteomyelitis or malignant bone tumors.

Through MRI examination, it is easy to mistakenly deem it as a large malignant tumor (upper left, center), yet the tumor is actually less than one centimeter (upper right)
Because osteoid osteomas are quite small, they are often worn out during surgery. We sometimes advise patients to take radiofrequency ablation, RFA, to burn the tumors. Hence, complete pathological specimens are often unavailable. Basically, under the microscope, we can see many immature woven bone tissues near the tumor. There will be lots of blood vessels, fibrous tissue, and scattering osteoblast and osteoclast in the' lesions nidus.' So there are abundant blood flows, and the nidus looks a little pink, which is very special! In addition, nerve fibers can be seen in tumors. Scientists also found high concentrations of prostaglandin and COX-1 and COX-II enzymes in tumors. All of the three hormones will stimulate the nerves and generate pains. This is why osteoid osteoma causes patients much pain, and the symptom improves immediately after taking painkillers
Osteoid osteoma won't incur lung metastasis!
by PQ Wu
Osteoid osteoma won't turn malignant!
by PQ Wu
The treatment of osteoid osteoma is important because the tumor can cause considerable discomfort in patients. Hence, active treatment to remove the tumor is very important. Two types of treatments for osteoid osteoma are currently available. One is surgical treatment, and the other is radiofrequency burning (RFA).
Traditional osteoid osteoma surgery is like breaking a butterfly on the wheel. Why? It is because osteoid osteoma has a very small size, and it hides in the bones. The surgeon couldn't identify the precise location of the tumor. Thus traditionally, the physicians would remove a large section of the bone, resulting in more bone defects and, therefore, the slower recovery of the patient. Another case is that the tumor is not handled since the surgeons couldn't see the tumor location, and the surgeons also have concerns about destroying too many bones. They can only grind more suspicious parts.
Because osteoid osteoma is really very small, and it hides in the bone, the surgeon in surgery simply can not see the correct location of the tumor.


Traditional surgery had to remove the entire bone to remove the tumor extensively.
Or, because of the concerns about destroying too many bones, the real tumor was not treated.

Therefore, in our Therapeutical and Research Center of Musculoskeletal Tumor in Taipei Veterans General Hospital, we collaborate with the Department of Radiology and use preoperative CT scanning to increase accuracy. The process is called "Mapping.", which is a quite brilliant approach.
Step 1: Work with a radiologist before surgery, and use computer tomography for precise positioning. Place a special needle near the tumor.


Step 2: After removing the needle, a hole in the bone can be used as a marker in operation.
Step 3: The orthopedic surgeon finds the hole during the operation.


Step 4: Use high-speed drills to remove tumors accurately and reduce damage to normal bones.
After surgery, because local bones are prone to bleeding, it is recommended to rest as much as possible one week after surgery and avoid too many intense exercises to prevent more bleeding and cause nearby tissue stickiness.
The second treatment is radiofrequency ablation (RFA).Radiofrequency ablation is operated by a radiologist. With CT positioning, the electrode needles are inserted into the tumor. Electrode needles release radiofrequency during treatment, generating heat in nearby tissues and burning tumors for coagulation necrosis. Radiofrequency ablation brings great effect to osteoid osteoma treatment! The only two drawbacks are that the NHI does not reimburse it, and the patients will need to pay lots of out-of-pocket expenses! In addition, because the tumor was burned directly, the correct biopsy results cannot be obtained. The patient may have some problems asking for reimbursement from private insurances.
Osteoblastoma is a very special bone tumor. The patients feel very uncomfortable, and it is not easy to diagnose clinically and treat accurately. It's a disease that bothers patients a lot!