Chinese: 外生骨疣、外生骨贅
English: Exostosis
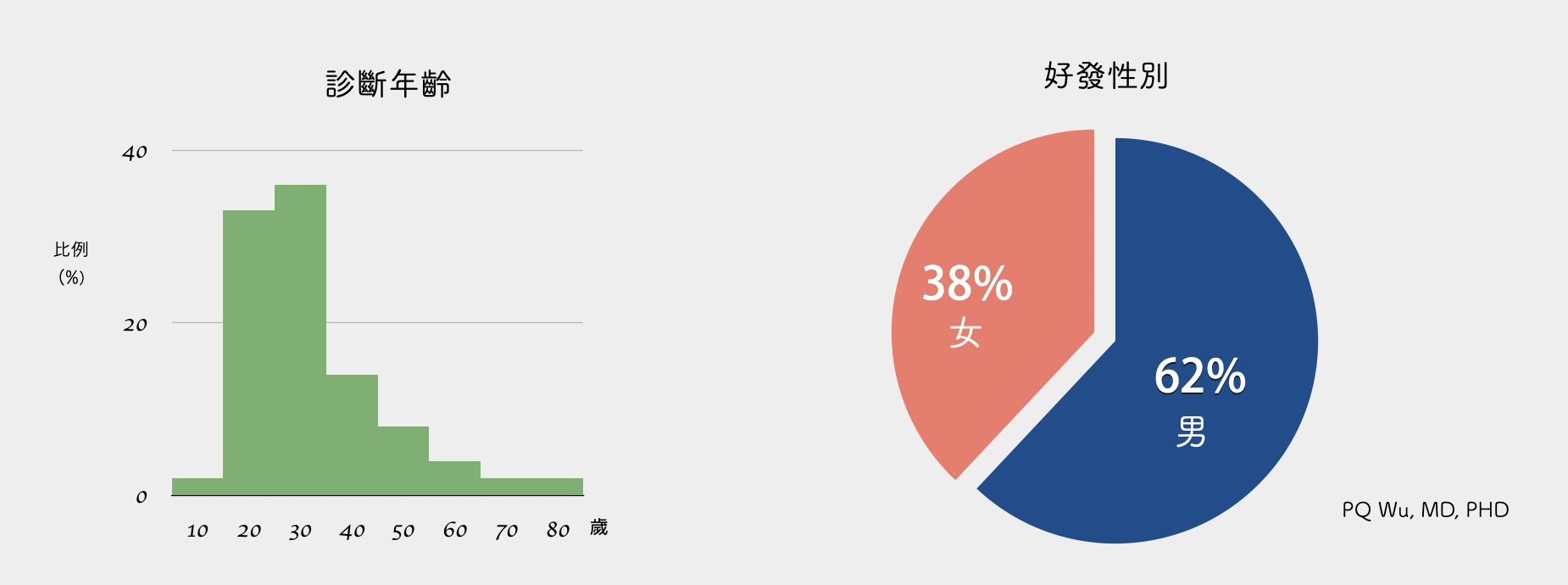
Osteochondroma is the most common benign bone tumor, taking about 33 to 45 percent in all benign bone tumors. Because the majority of osteochondromas have no symptoms, they will not be examined and diagnosed. Hence, the exact incidence of osteochondroma is unclear. Approximately, one in 200 teenagers will have a chance of occurrence.
Osteoblastoma has a higher chance to occur in men, accounting for about 60%. Most of these occur in adolescents between the ages of 10 and 20. About 60 percent of patients have osteochondroma surgically removed before the age of 20.
1. Growth plate injury.
2. Protruding from the bone.
3. Bones and cartilage grow gradually.
4. Formation of osteochondroma
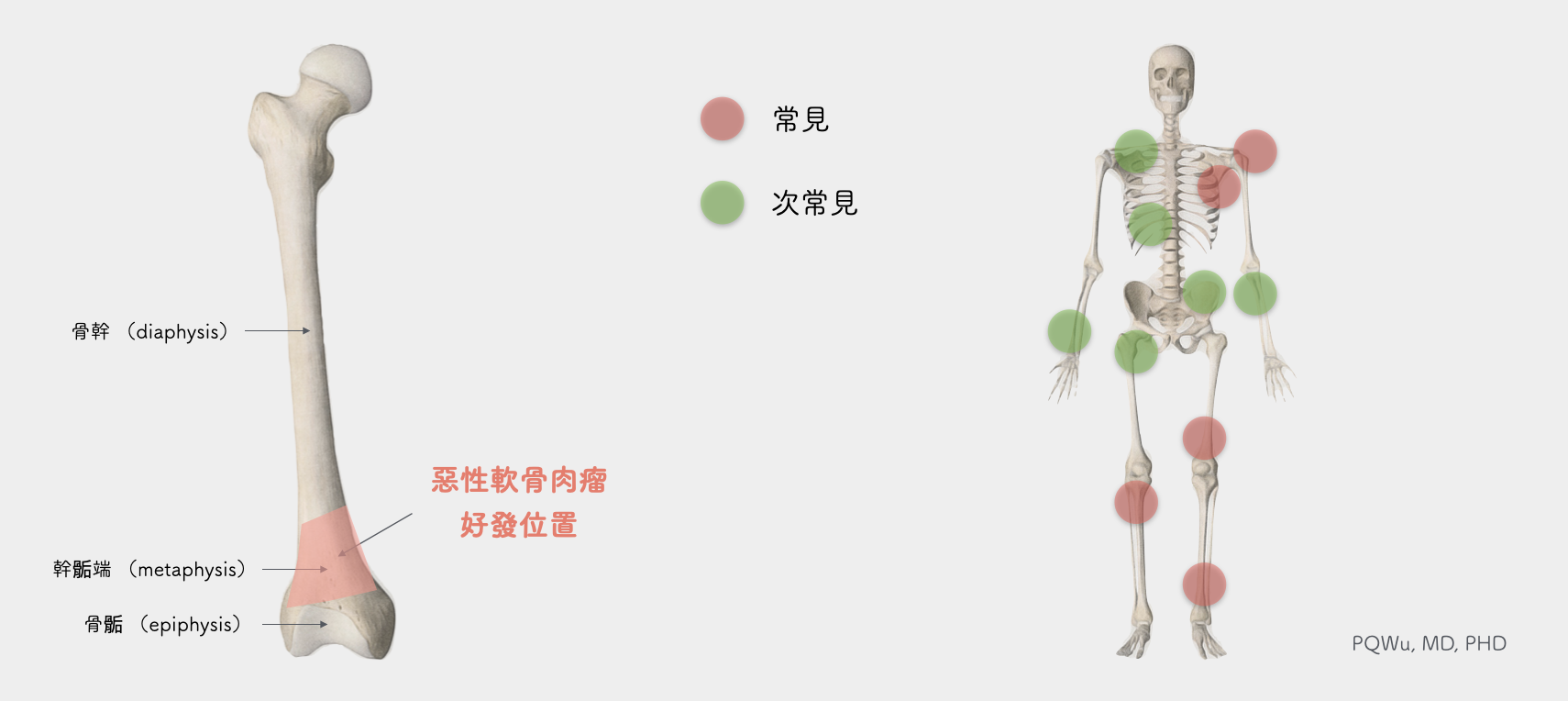
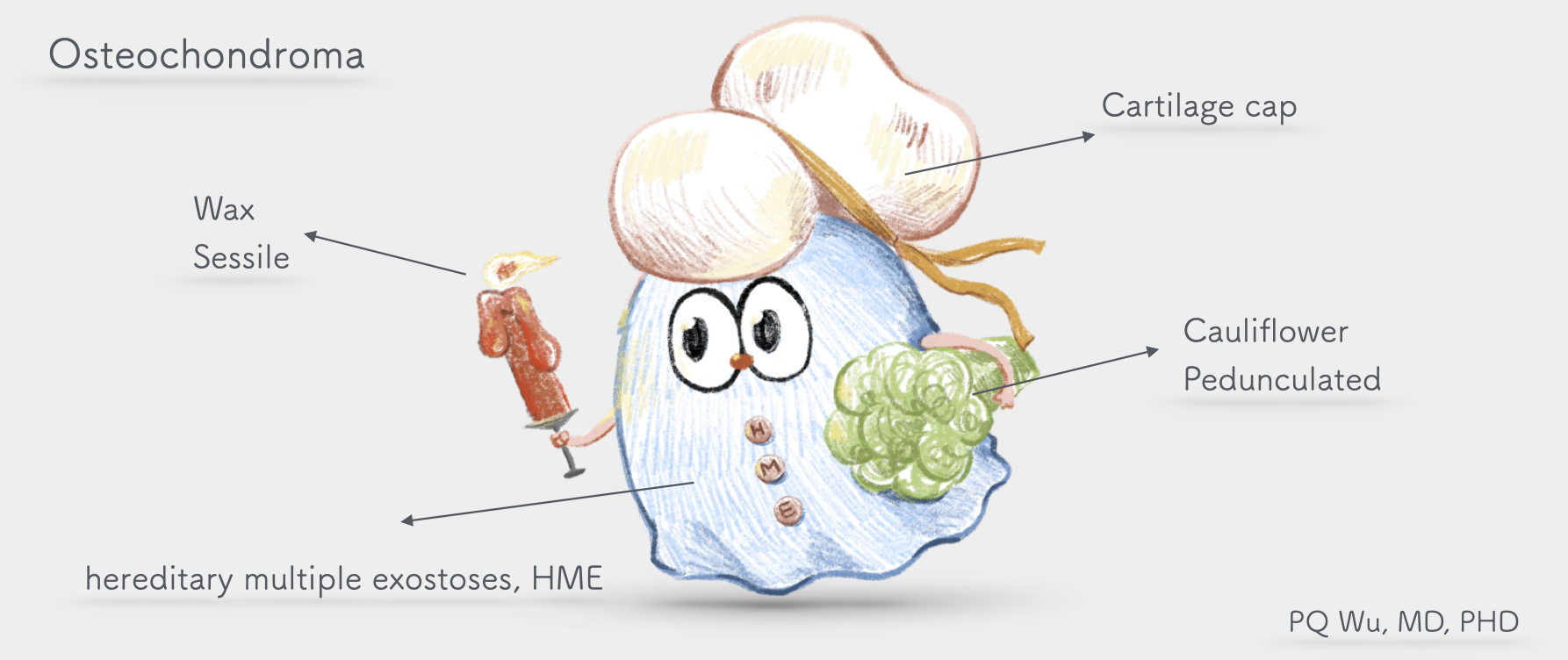
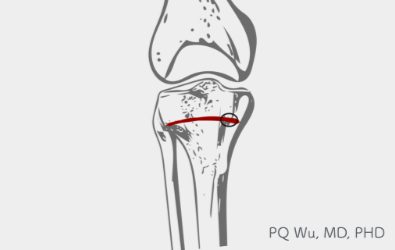
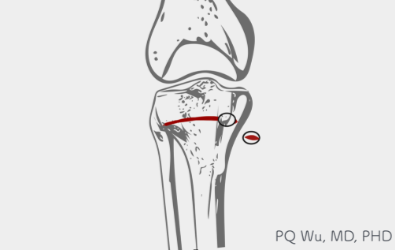
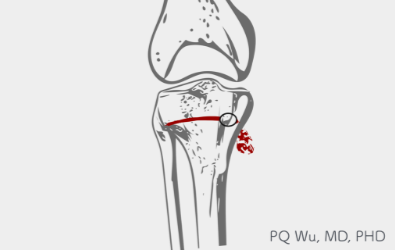
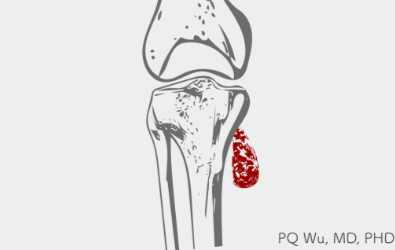
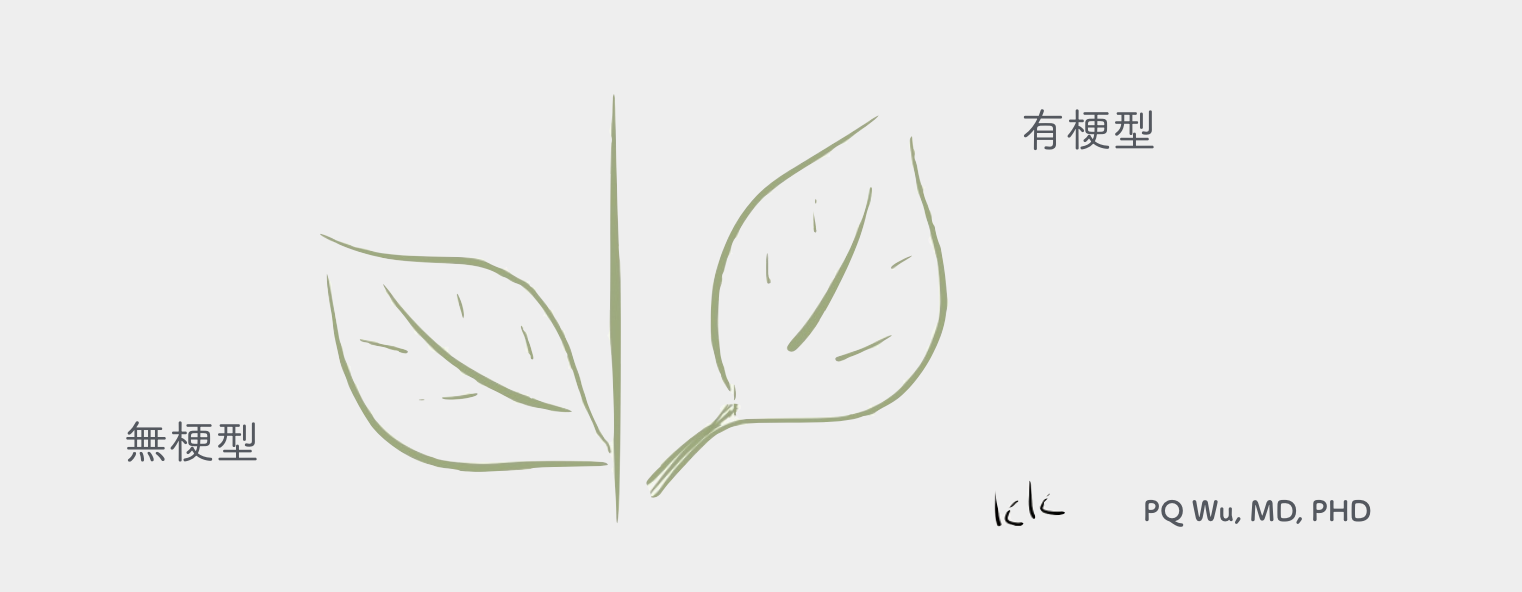
Under X-rays images, we can observe an osteochondroma tumor grow from the edge of a normal bone, as leaves grow from a branch. We can classify it into Sessile and Pedunculated osteochondroma.
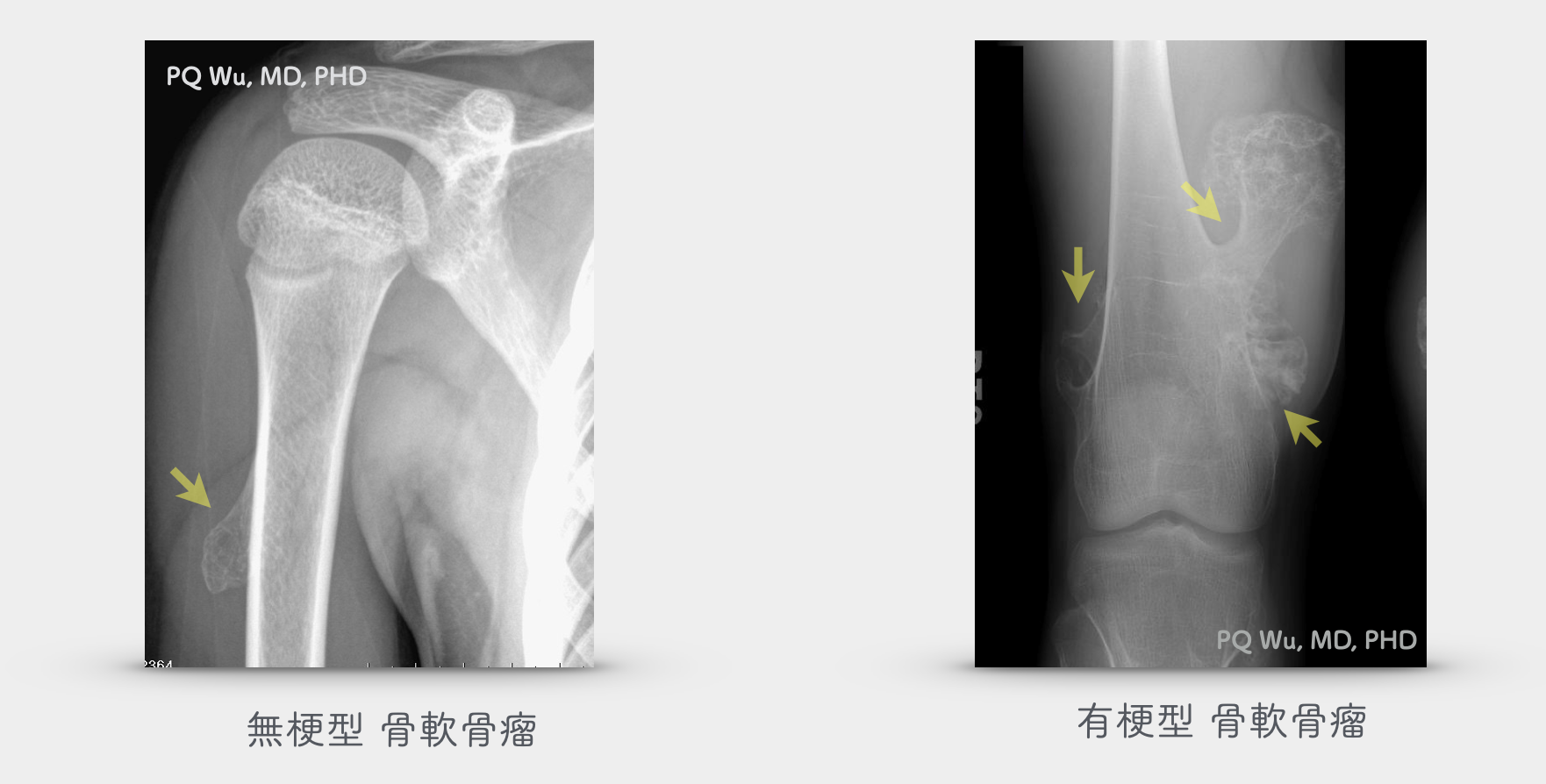

Sessile Pedunculated osteochondroma

Pedunculated osteochondroma
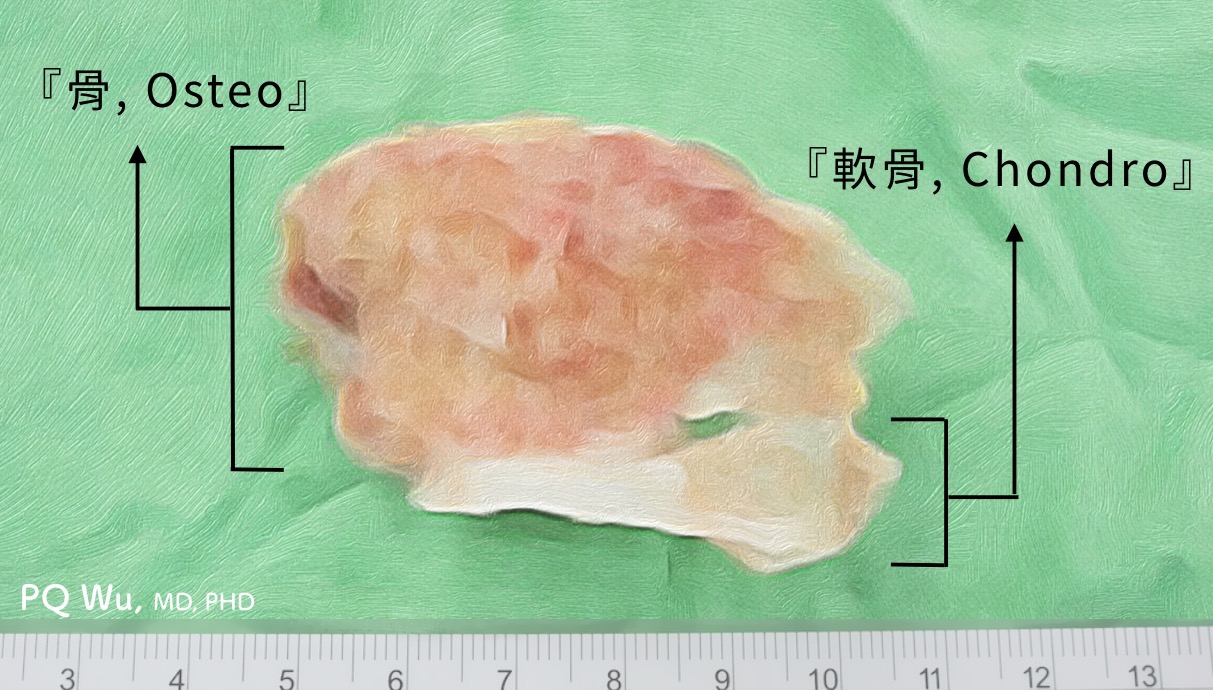
Osteochondroma, as the name suggests, is a tumor made up of 'bone- Osteo' and 'cartilage- Chondro'. The 'cartilage' component will cover the bone like a hat; hence, we will call it 'Cartilage Cap.' Because cartilage is not visible under X-rays, the actual size of the tumor is larger than the size measured under X-rays. The cartilage cap plays an important role in pathologic diagnosis and imaging examination. The regular cartilage cap is about 2 to 3mm thick and has a smooth surface. However, in children and young people who are growing up, the thickness may increase. Notably, if the thickness of the cartilage cap in the adult is found greater than two centimeters, and the cap surface is uneven, rough, and even has 'cystic change,' we should be mindful of the possibility of whether it turns into malignant chondrosarcoma.
Most of the osteochondromas are single lesions, and only about 15% are multiple. Those multiple lesions are medically referred as multiple osteochondromatosis or hereditary multiple exostoses, HME. In 90% of patients with multiple osteochondromas, we find germline mutations in their EXT1 or EXT2 gene.
Osteochondroma does not incur lung metastasis.
It's possible, and the average chance is 3%.
In current studies, the probability that osteochondroma will turn into malignancy varies a lot since the selections of patient samples are different.
I. In a study published in 1982in the medical journal- Cancer, David Dahlin, a reputed pathologist at Mayo Clinic, found that 27.3 percent of multiple osteochondromas turned malignant in the patients who seek surgical treatment, while only 3.2 percent of single osteochondroma turned malignant in the patients who seek surgical treatment.
II. According to a statistical study published by Dr. Peterson in 1989, only about 1% of multiple osteochondromas turned malignant afterward.
III. A 2011 study by the Royal Infirmary of Edinburgh found that out of 172 cases of shoulder multiple osteochondromas, seven turned into malignant, or 4 percent. The study also found that when patients had mutations in their EXT1 gene, their osteochondromas were more likely to become malignant.
The differences should be caused by the patients taking the initiative to seek medical treatment since pains occurred when their osteochondromas turned malignant. Hence, the possibility of having malignant transformation is higher in the former studies.
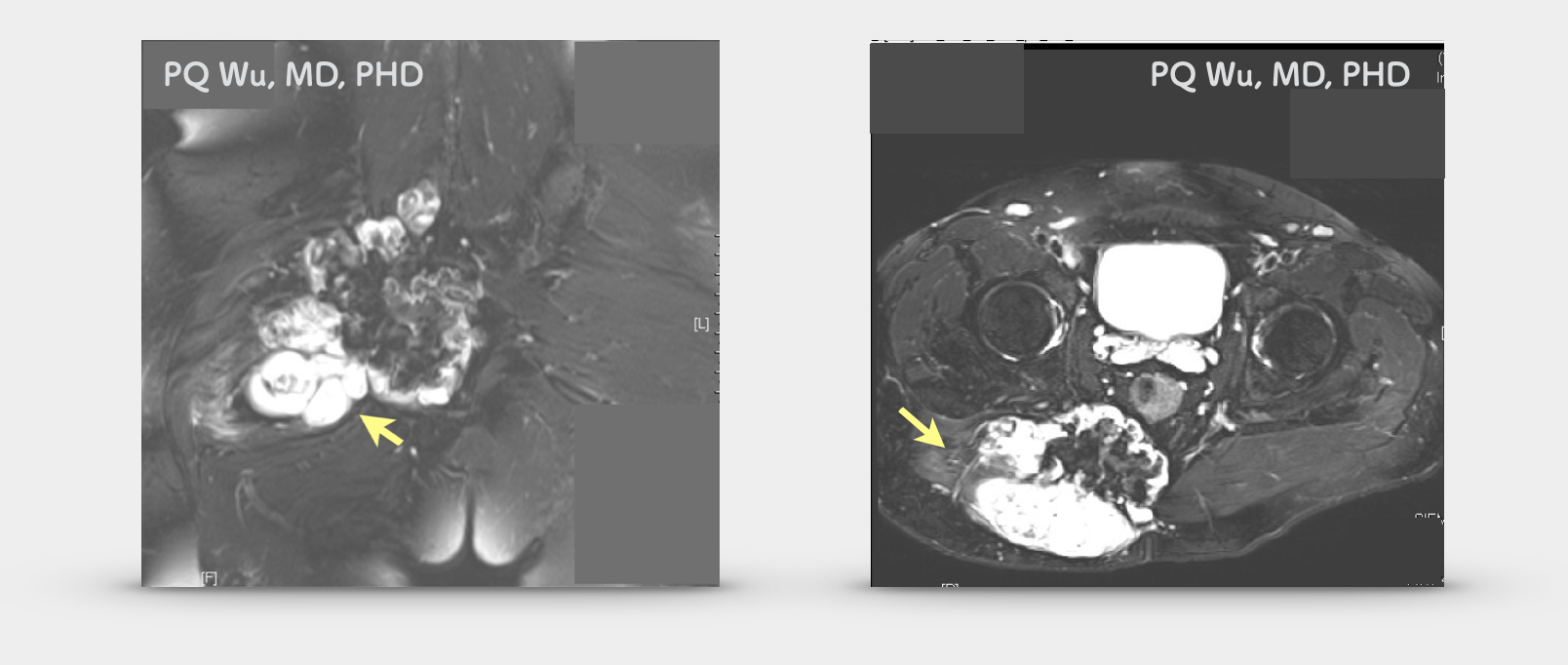
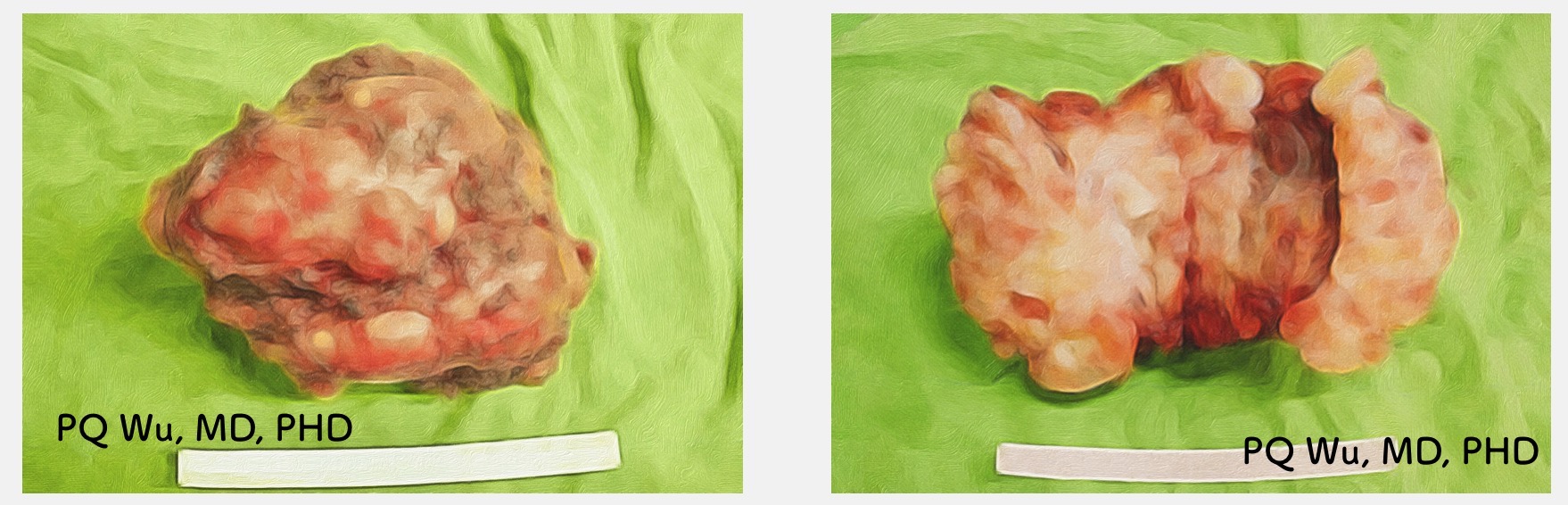
An 18-year-old male whose multiple osteochondromas turned into severe malignant osteochondroma.
Surgical Principles of Osteochondroma
Must conduct surgical removal
Tumor volume continues increasing after turning adult
Night pain
Recommended for surgical removal
Tumor presses nearby soft tissue and/or bone
Tumor grows at the axial skeleton
No need for surgical removal
Asymptomatic
(a) Must conduct surgical removal
We will ask the patients to consider removing their tumors if they have the following two symptoms, which may raise the concern of turning malignant and send the tumors to pathology examination.
1. Tumor volume continues increasing after turning adult.
Theoretically, osteochondroma should stop growing when we stop growing. Hence, if the tumor continues to grow after a patient turns 18, special attention must be paid.
2. Night pain
Night pain or resting pain unrelated to activity occurs. Theoretically, osteochondroma itself will not be painful unless, as mentioned earlier, the tumor presses the nearby tendon or other soft tissue, leading to the experience of pain and discomfort to the patient during activity. Or, a fracture caused by the impact at the osteochondroma site will cause pain. However, if these are not the cases, and the patient has no special activity or injury recently, the osteochondroma originally steady suddenly develops night pain or resting pain will require special attention

(b) Recommended for surgical removal
1. The tumor presses nearby soft tissue
Osteochondroma presses the nearby soft tissues, resulting in active pains. These pains affect the quality of life and prevent the patients from doing normal exercise.
2. The tumor presses nearby bones
Osteochondroma presses nearby bones, resulting in limb deformations. Especially for those close to the joint surface, joint damages and other sequelaes will likely occur afterward if the deformations continue.


3. Tumor grows at the axial skeleton
Osteochondroma grows at the axial skeleton, such as the spine, pelvis, etc. As mentioned earlier, osteochondroma, which grows at the axial skeleton, has a higher chance of turning malignant
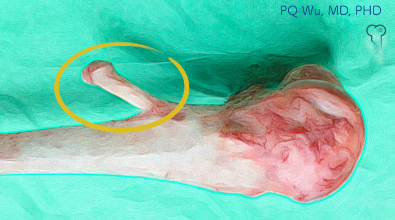
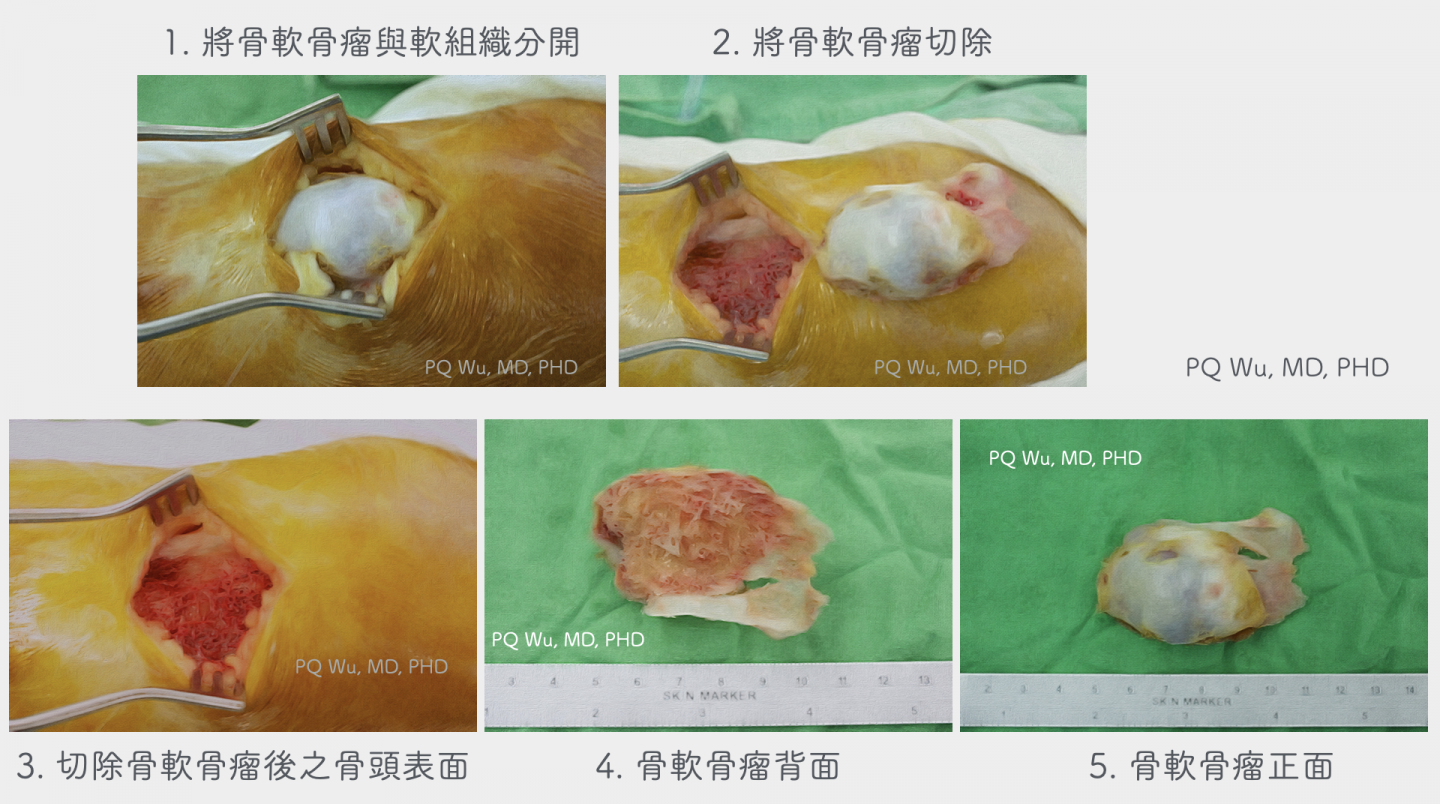
In the surgical procedure, the orthopedic surgeon will first separate the tumor from the nearby soft tissues, use an osteotome to shovel the tumor, and then use X-ray scanning to confirm any residual tumor. Usually, the operation should be over within an hour. However, if the tumor grows in a special position and is close to important nerves or vessels, the surgery time and risk will increase a lot. The following are pictures of our surgery:
After the surgery, because local bones are prone to bleeding, the patients will be recommended to rest as much as possible one week after and avoid much intense exercise to prevent more bleeding and nearby tissue stickiness. Generally, we will advise patients, if they really need it, to try to come during winter or summer vacation time for surgery so that after the surgery, they will be able to rest fully.